The Mind-Body Connection
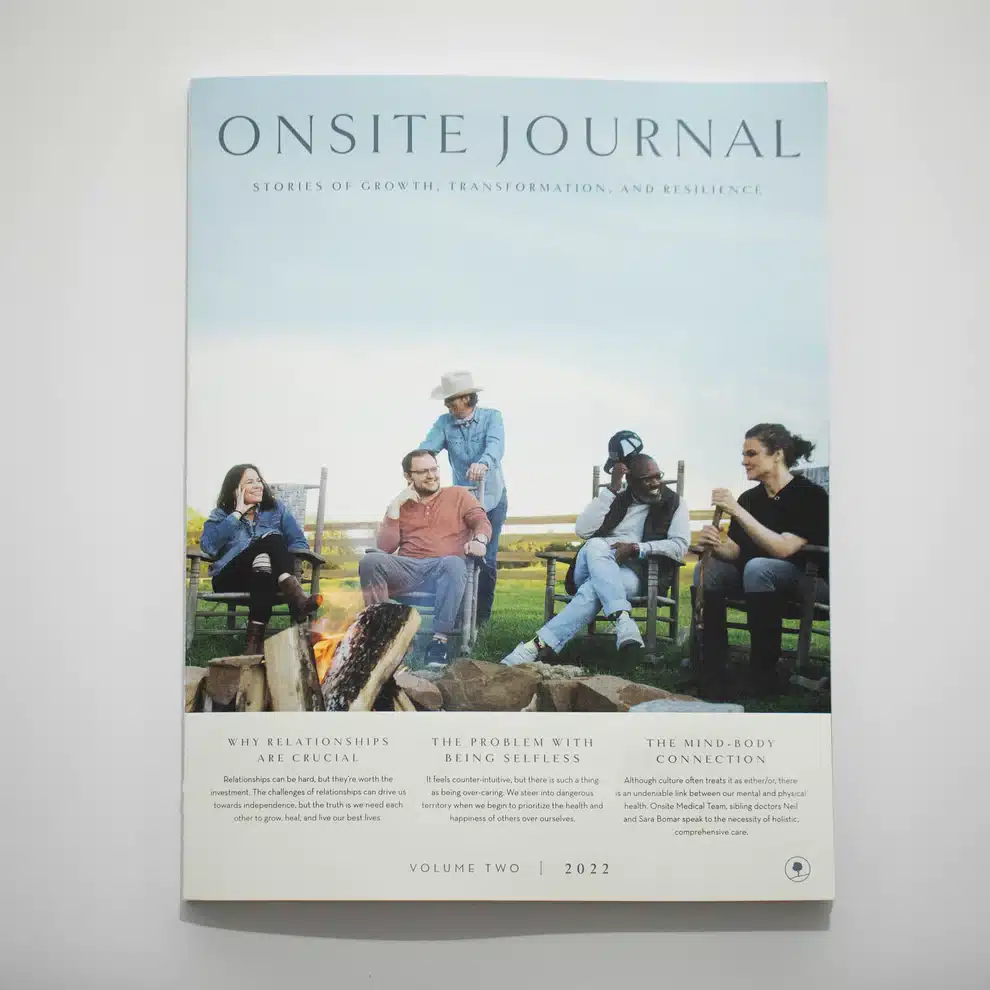
Excerpt from The Onsite Journal Volume II
Mickenzie Vought sits down with Onsite’s Sibling Duo, Doctors Neil and Sara Bomar
Most traditional models of medicine approach the mind and the body as separate entities. As a result, we see one doctor for our physical ailments and another to address mental and emotional struggles. At Milestones, we believe it’s important to think more holistically about your health.
We brought in two experts with different disciplines to offer their perspectives into the complex and intrinsic mind-body connection.
With their unique approaches and specialties, siblings psychiatrist Dr. Neil Bomar and functional medicine practitioner Dr. Sara Bomar play a vital and unique role for clients of Milestones, Onsite’s Residential Trauma Program by partnering to provide comprehensive, holistic care. Onsite Editorial Director, Mickenzie Vought (MV) sat down with the two to better understand the mind-body connection that informs and influences the way they approach their clients and the advice they’d have for us all as we seek to have a more holistic approach to our health.
MV: I would love for people to get to know you a little bit. Dr. Sara, can you tell me a little bit more about your role as a functional medicine doctor?
SARA: In my functional medicine practice, I do a much deeper dive into a patient’s health issues than one would typically have in a traditional doctor’s visit. While I have traditional medicine training and accreditation, I additionally have the benefit of being able to incorporate supplements and other integrative measures to figure out all of the ways to treat my patients. I love being able to step back, see the bigger picture, connect the dots, and uncover the root causes of what is making people sick.
MV: How did you personally discover and begin working with people to connect the dots between their physical symptoms and their emotional pain?
SARA: There’s nothing that teaches you to be a better practitioner than being a patient. Several years ago I was suffering from the symptoms of a rare spinal condition called arachnoiditis, and it took eight years for someone to diagnose it adequately.
My symptoms got so bad that I was confined to a wheelchair with inflammation throughout my body, and I had a hunch that it was all connected. So here I was, a trained physician asking deeper questions, wanting some additional nontraditional resources, and researching the realm of functional medicine. As a result of that, I was able to uncover new treatment options.
Ultimately, what was supremely helpful was stem cells. When I went in for my stem cell treatments, the doctor was amazed at my already bolstered stem cell count. Supplements, diet, and community sup- port were the grid on which other treatments could be built upon. After my recovery, I decided to go back and get trained in functional medicine through Cleveland Clinic.
NEIL: After 14 years of being in a wheelchair, Sara deciding to turn to an alternative and complementary field of medicine to heal herself was a wake-up call for both of us. When she went through training in functional medicine and began to show me these peer-reviewed articles in scientific journals, it gave credence and credibility to the field and practices, and we began to work together on treating some of the patients I was seeing in my psychiatric practice.
If I were a patient, I would rather have two sets of eyes looking at me than one. Dr. Sara looks at how people’s symptoms impact their stories, and I tend to look at how people’s stories impact their symptoms. Bringing these two perspectives together creates a unified whole in how we treat clients.
MV: Dr. Neil, you had a unique journey to the practice of psychiatry. Can you share what led you to this field of medicine?
NEIL: For me, autonomy and freedom are everything. My early career in occupational and preventive medicine lacked a lot of creativity. I began to rethink my life, like a lot of people, after 9/11. I decided I wanted more in my work. I wanted to become a psychiatrist. The first week of my residency, I felt like I finally was home. It’s what I am meant to do. Understanding a person’s whole story is very important to me, and seeing people get better is my jam. I’ve done child and adolescent psychiatry, I’ve done alcohol and drug treatment, I’ve done geriatric psychiatry, and now, I’m a trauma psychiatrist here at Onsite. At Milestones, we’re able to give curated, individualized care to each person. I cannot believe I get to practice this type of medicine. I tell people all the time, “I am the luckiest psychiatrist in the universe.”
MV: You guys work together in such a beautiful way to care for the clients of Milestones. Based on that work, what do you each wish people knew about the connection between their mental and physical health?

NEIL: Historically, the brain and the body have been considered two separate entities. And fortunately, now, as we’re stepping into a new era of research in neuroscience, we know that that’s not the case. One of the most intriguing connections that I work on with Dr. Sara is the gut-brain connection. The more I read about it, and the more I see the research, the more I want everyone to understand it. Studies show the importance of the gut microbiome, feeding your gut, and healing your gut. Our gut effects our brains, specifically related to how we process feelings of depression and anxiety.
There are so many other drivers of anxiety and depression than we previously thought. For example, we now can do a quick, painless genetic test to see how people metabolize B vitamins. Did you know that most people with depression have an inborn genetic error that inhibits their ability to metabolize B vitamins? The good news is we can now easily detect that deficiency and adequately replace that with supplements instead of medicines that would treat the symptoms and not the cause.
Also, did you know that inflammation is the foundation for most disease processes, including depression? When we’re able to dig into a client’s chemistry, and when we’re able to find sources of inflammation and correct them, healing follows.
SARA: Mainstream practitioners tend to just hear you’re depressed and are quick to prescribe an antidepressant. They often neglect to see the connections and dig into the root problems.
I wish both patients and physicians had the foresight to separate the two, our mental and physical symptoms and health.
Anybody who experiences chronic pain knows frustration and fatigue. So as a practitioner, I create space for my patients to discuss all sorts of things in the mental health realm that we know will impact their physical health and vice versa. I would encourage people to speak up, whether they’re talking to their therapist about their medical issues or talking to their medical doctor about their emotional issues. They are all interrelated and interdependent.
MV: The work and research of Dr. Bessel van der Kolk and The Body Keeps the Score first introduced many of us to the physical- mental connection. In your work, how have you seen unresolved trauma impacting people’s physical health?
SARA: There’s a well-known correlation between trauma and illness. For example, we’ve seen from adverse childhood experience (ACE) studies that kids with higher adverse life experiences are at risk for autoimmune disease, obesity, heart disease, etc.
NEIL: So many autoimmune disorders come from unresolved trauma. Research shows that early adverse childhood experiences change the gut microbiome—the bacteria in your gut. Survivors of trauma, even in adulthood, can have an abrupt change in their gut microbiome. It’s incredible.
SARA: There are studies of the differences in health of the gut microbiome in people who have experienced trauma versus people who have not experienced significant trauma. We also know that cardiovascular disease has an inflammatory component and trauma increases those inflammatory cytokines.
MV: Neil, how has your work at Milestones impacted the way you practice psychiatry?
NEIL: Professionally, I have to rely on medications in many cases. But when a client can come in and devote time, energy, and lifestyle change to their regimen, so many times, I’m able to practice psychiatry by subtraction. Meaning, often at Milestones, I’m able to take people off more medicine than I put them on. When they get into a healthy, vulnerable healing community, detox from electronics, get on a schedule with adequate sleep and diet, and receive world- class therapeutic services, they’re shocked to find out all of those things together combine to improve their health.
MV: I love that it’s not one thing but a holistic regime that brings about the most significant shifts. Dr. Sara, after reading this article, I would expect many people to want to learn more about functional medicine and be looking for a functional medicine doctor. Is there a resource that you recommend to people to get connected with a practitioner in their area?
SARA: When searching for functional medicine practitioners, I like to look at Cleveland Clinic’s Institute for Functional Medicine because they have a certification process. I know the training that they’ve had, and there’s a measure of confidence in that.
MV: As we wrap up, I would love to leave people with a few practical things to start this journey. Dr. Neil, from your experience, what supplements can we integrate to impact our mental health?
NEIL: Vitamin D, Methylated B vitamins, and omega-3 fatty acids, usually in the form of fish oil. At Milestones, I would estimate that 80% of our clients have a low vitamin D level, which can have drastic impacts on mental health. I mentioned the connection between absorption of B vitamins and depression—omega-3 supports our brains that are nearly 60 percent fat.
MV: Thanks for those recommendations! Dr. Sara, in your experience, what are some things you’d recommend we all do to care for ourselves holistically?
SARA: As a general rule, I would recommend the same three supplements and additionally include Vitamin K and a good multivitamin.
If you have medical clearance, exercise is one of the most significant ways to impact our emotional health positively. There has been study after study about the ability to increase the number of mitochondria in the brain with exercise. Mitochondria are essential because they’re the cell’s battery; that’s what energizes that cell and enables it to do what it needs to. In addition, there are so many other benefits in self- image, vitality, sex drive, and a whole host of things.
And second is diet. In general, a diet that is low in sugar and high in non-starchy vegetables (with a lower glycemic index), and incorporates proteins or meats that have been responsibly raised—alongside being high in omega-3s—will benefit 95% of folks out there.
Hear more the Drs. Bomar on The Treating Trauma Podcast

NEIL BOMAR, MD
Milestones at Onsite Medical Services Director and Psychiatrist
Dr. Neil Bomar has a varied medical and psychiatric background. He is an honors graduate of Vanderbilt University and completed his medical degree at the University of Tennessee Health Sciences Center in Memphis. An early career in primary and urgent care medicine led him to Kentucky, where Neil attended the University of Kentucky to pursue a residency in occupational and preventive medicine. He practiced occupational and corporate medicine before returning to Memphis to complete a residency in psychiatry.
Neil’s breadth of experience in psychiatry and primary care led to a focus in the areas of trauma and addiction. He now serves as the Medical Services Director for Milestones, Onsite’s Residential Trauma Program in Cumberland Furnace, TN

SARA BOMAR, MD
Milestones at Onsite Adjunct Physician and Functional Medicine Doctor
Dr. Sara Bomar scored in the top 7% of all physicians in the nation on her medical boards when graduating from Meharry Medical College. While working as a resident physician in a highly competitive residency at Vanderbilt Hospital, Dr. Bomar developed a back injury expected to respond to a fairly routine surgery. Instead, rather than recovering, she became more and more debilitated. It would take eight years to receive a correct diagnosis and yet six more years for a treatment that would allow her to walk again and live with significantly less pain. Sara’s journey forever changed the way she would practice medicine.
Now running her own functional medicine practice, Dr. Bomar works day in and day out, helping individuals find the root causes of illness and implementing changes at those roots.

More resources from Milestones